By Tony Pugh, McClatchy Washington Bureau
WASHINGTON — As procrastinators rushed to buy health insurance Monday by the Affordable Care Act’s official enrollment deadline, new research estimates that about half of those with subsidized coverage obtained from federal or state marketplaces will lose it within a year because of changes in their incomes or other family circumstances, such as divorce, relocation or the births of children.
The same is true for about half of new Medicaid recipients, who are likely to lose program eligibility at some point over the next year for a variety of reasons, said Benjamin Sommers, an assistant professor of health policy and economics at the Harvard School of Public Health.
When people lose, drop or change health coverage for unforeseen reasons, it’s known as “churning.” It’s a common occurrence for consumers with individual coverage bought outside the workplace, as well as for those with Medicaid, the state-federal health program for poor people and those with disabilities.
Along with being a bookkeeping headache for insurers and Medicaid administrators, churning undermines the continuity of care between doctors and patients by causing patients to miss treatments and sometimes seek new caregivers.
It also has a financial impact, as coverage lapses may lead to costly emergency room visits when primary physicians could have provided treatment for far less.
In the 25 states that expanded eligibility for Medicaid under the Affordable Care Act, churning probably won’t leave people without coverage because there’s no gap between the income thresholds for Medicaid and subsidized marketplace coverage. Instead, millions will move between eligibility for both as their incomes are periodically updated and verified.
“It’s not exactly that they’ll lose coverage,” Sommers said in an interview. “It’s that they may have to change the coverage they have.”
But for people in states that so far have declined to expand Medicaid, “then they’re worse off,” he said. If they lose their eligibility for subsidized coverage when their incomes fall too low to qualify, “they will probably have no option for coverage,” Sommers said.
That’s because the income limits to qualify for Medicaid in non-expansion states are far below the levels at which subsidized marketplace insurance is available. That creates a “coverage gap” in which millions of people earn too much to qualify for Medicaid but not enough for federal subsidies to help them buy marketplace insurance.
“In other words, most adults who lose marketplace subsidies in non-expanding states will become uninsured,” Sommers and three other researchers wrote in their report on churning in the April edition of Health Affairs magazine.
Expansion states with lower poverty rates and higher per-capita incomes will see more churning because they have more adults with incomes near the eligibility line for Medicaid and subsidized coverage, Sommers said in the interview.
Half of Americans with individual health insurance churned in and out of coverage in 2010, according to recent congressional testimony by Medicaid Administrator Marilyn Tavenner. The reasons were myriad: Some couldn’t afford it, some switched to different plans and others may have dropped their coverage after obtaining job-based insurance.
The average Medicaid recipient loses coverage for 20 percent of the year — nearly 10.5 weeks — because of administrative violations, clerical errors, income changes or other factors that make him or her ineligible, according to researchers at George Washington University.
“The implication is that eligibility changes are likely to be a major challenge for every state as implementation of the ACA continues,” according to the Health Affairs article.
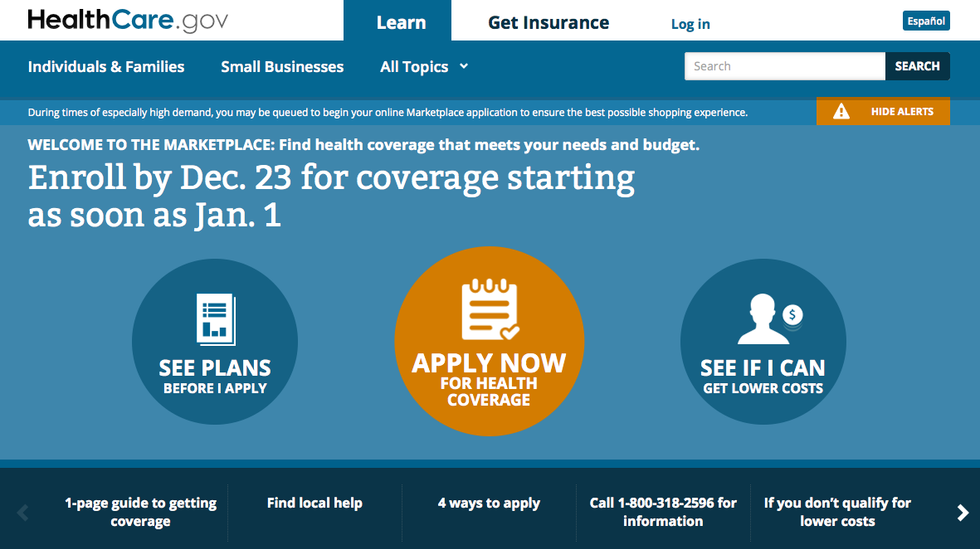
Photo via HealthCare.gov


