Even After Open Enrollment, Activity Remains Unexpectedly High On Federal Health Insurance Exchange
by Charles Ornstein,ProPublica
This story was co-published with NPR’s “Shots” blog.
For months, journalists and politicians fixated on the number of people signing up for health insurance through the federal exchange created as part of the Affordable Care Act. It turned out that more than 5 million people signed up using HealthCare.gov by April 19, the end of the open-enrollment period.
But perhaps more surprising is that, according to federal data released Wednesday to ProPublica, there have been nearly 1 million transactions on the exchange since then. People are allowed to sign up and switch plans after certain life events, such as job changes, moves, the birth of a baby, marriages and divorces.
The volume of these transactions was a jolt even for those who have watched the rollout of the ACA most closely.
“That’s higher than I would have expected,” said Larry Levitt, senior vice president for special initiatives at the Kaiser Family Foundation. “There are a lot of people who qualify for special enrollment, but my assumption has been that few of them would actually sign up.”
The impact of the new numbers isn’t clear because the Obama administration has not released details of how many consumers failed to pay their premiums and thus were dropped by their health plans. All told, between the federal exchange and 14 state exchanges, more than 8 million people signed up for coverage. A big question is whether new members will offset attrition.
ProPublica requested data on the number of daily enrollment transactions on the federal exchange last year under the Freedom of Information Act because the Obama administration had declined to release this information, a key barometer of the exchange’s performance, to the public. The administration also has not put out any data on the exchange’s activity since the open enrollment period ended.
The data shows so-called “834” transactions, which insurance companies and the government use to enroll new members, change a member’s enrollment status, or disenroll members. The data covers the 36 states using the federal exchange, which include Texas, Florida, Illinois, Georgia and Michigan.
When HealthCare.gov rolled out last fall, insurance companies complained that the information in the 834s was replete with errors, creating a crisis at the back end of the system.
Between April 20 and July 15, the federal government reported sending 960,000 “834” transactions to insurance companies (each report can cover more than one person in the same family). That includes 153,940 for the rest of April, 317,964 in May, 338,017 in June and 150,728 in the first 15 days of July. The daily rate has been fairly stable over this period.
It was not immediately clear how many of the records involved plan changes or cancelations and how many were for new enrollments.
An insurance industry official estimated that less than half of the transactions are new enrollments. The rest are changes: When an existing member makes a change to his or her policy, two 834s are created — one terminating the old plan and one opening the new one.
Charles Gaba, who runs the website acasignups.net that tracks enrollment numbers, estimates that between 6,000 and 7,000 people have signed up for coverage each day on the federal exchange after the official enrollment period ended. Gaba’s predictions were remarkably accurate during the open enrollment period.
“That doesn’t account for attrition. That doesn’t mean that they paid,” Gaba said. “That’s been based on limited data from a half dozen of the smaller exchanges, extrapolated out nationally.”
The federal data obtained by ProPublica confirm some other facts about the rollout of HealthCare.gov, which was hobbled initially by technical problems. The slowest day was Oct. 18, when no 834 transactions were sent. That was followed by Oct. 1, the day the website launched, when a grand total of six records were sent to insurers.
By contrast, the busiest day was March 31, the official end of open enrollment, when 202,626 “834” reports were sent to insurers. The entire last week in March was busy.
About 86 percent of those who signed up for coverage on the federal exchange were eligible to receive government subsidies to help lower their monthly premiums. Those subsidies are being challenged by lawsuits in federal court contending they aren’t allowed by the Affordable Care Act.
Two federal appeals courts came to conflicting decisions Tuesday on the permissibility of the subsidies (one said yes; the other no). They will remain in effect as the cases proceed in the courts, the Obama administration said.
The next time that the general public can sign up for coverage through the exchanges is from November 15 to February 15, 2015.
Click here to download the data (Excel or CSV) released to ProPublica under the Freedom of Information Act.
Read our previous coverage of the Affordable Care Act and share your story.
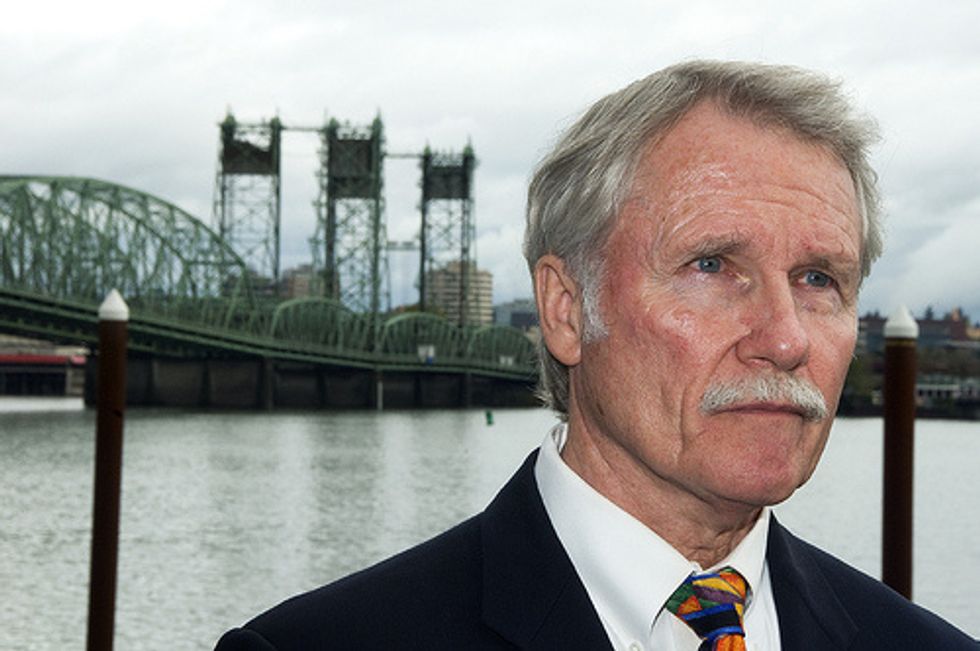
AFP Photo/Joe Raedle