By Blythe Bernhard, St. Louis Post-Dispatch (TNS)
ST. LOUIS – Is the best treatment for cancer already inside of us? Research is underway at Washington University to test a new approach to cancer treatment. Beyond traditional therapies like surgery, chemotherapy and radiation, scientists want to know if the human body’s own immune system can attack tumors.
They’re testing personalized vaccines designed to target deadly cancer cells in each patient. A vaccine is any substance that prevents or treats a disease with properties of the disease itself. Scientists know that fighting fire with fire works for many viruses like flu, measles or polio. Now they want to test that theory with cancer, but since every tumor is different, every vaccine will be different.
Advancements in genetic sequencing, or decoding the DNA of cells, have made it easier to figure out what makes tumors unique. Scientists have found potential targets in tumor cells that could cause them to break down. Now they’re passing that knowledge on to doctors to try out in their patients with the most challenging cancers. Clinical trials are now enrolling patients with melanoma, brain cancer and breast cancer.
The concept is hypothetical. The research is experimental. There is no proof that it works.
But after staring down deadly cancers, tumors that have spread, and patients who are out of options, doctors are intrigued.
For decades, scientists have gone back and forth on whether the immune system – the body’s defense mechanism – has anything to do with cancer. In the 1950s a concept called cancer immuno-surveillance took hold, meaning that the immune system could recognize tumor cells as foreign. By the 1970s the theory was rejected after laboratory mice with weak immune systems did no worse than normal mice when they developed cancer.
Most cancer scientists moved on to trying different pharmaceutical routes for new treatments. Robert Schreiber of Washington University wanted to know more about those mice. He started more sophisticated tests with mice that lacked a critical gene that allowed the immune system to make lymphocytes – white blood cells that defend the body against disease.
“What we showed conclusively was mice that had defects in the immune system got tumors more quickly and in higher incidences than normal mice,” Schreiber said.
And with that, the concept of cancer immunology was back. The Center for Human Immunology and Immunotherapy Programs at Washington University launched last year with Schreiber as director to help doctors use the immune system to fight cancer and other diseases.
Other medical centers around the world have taken different approaches to cancer immunology. Duke University is working with a polio virus vaccine to induce the immune system to fight brain tumors. The Mayo Clinic is doing a similar trial with a measles vaccine. Other clinical trials involve reprogramming the immune system’s checkpoints that prevent it from attacking certain cells.
Washington University leads the study of personalized cancer vaccines. With help from their genetic sequencing labs, local scientists try to isolate the best antigen targets – or the most dangerous mutated cells – from each patient’s tumor to vaccinate against.
Vaccines are typically viewed as preventive, such as flu shots to help avoid flu infection. Cancers known to be caused by viruses can also be prevented this way. The HPV (human papillomavirus) vaccine can prevent some cervical cancers and the hepatitis B shot protects against development of liver cancer caused by that virus.
Scientists now think vaccines can also be used to stimulate the immune system to fight cancers that are already formed. But without a known virus or other cause, scientists must figure out what differentiates a patient’s tumor cells from healthy cells. Then they must try to vaccinate against mutations, called neo-antigens that occur only in the bad cells.
The immune system is a finely tuned machine that is difficult to manipulate. One challenge is turning up a patient’s immunity without harming healthy cells, the process that happens in autoimmune disorders like multiple sclerosis. One type of immunotherapy, called checkpoint blockade, is risky because it can backfire and make the patient vulnerable to an overly aggressive or weakened immune response. Cancer vaccines, in theory, could be safer because they activate more highly precise targets.
“The real essence of that vaccine design is picking out the peptides (proteins) that have the strongest interaction with the patient’s immune system,” said Elaine Mardis, director of technology development at the university’s McDonnell Genome Institute. “It’s a different answer for every patient.”
Melanoma
The first human trial to apply this concept included three patients with melanoma whose cancer had spread to their lymph nodes. After surgeries to remove their tumors, their cancerous and healthy cells were sequenced to identify mutations. The patients received an infusion using cells from their own immune systems. The treatments stimulated the immune system through a boost of protective T-cells.
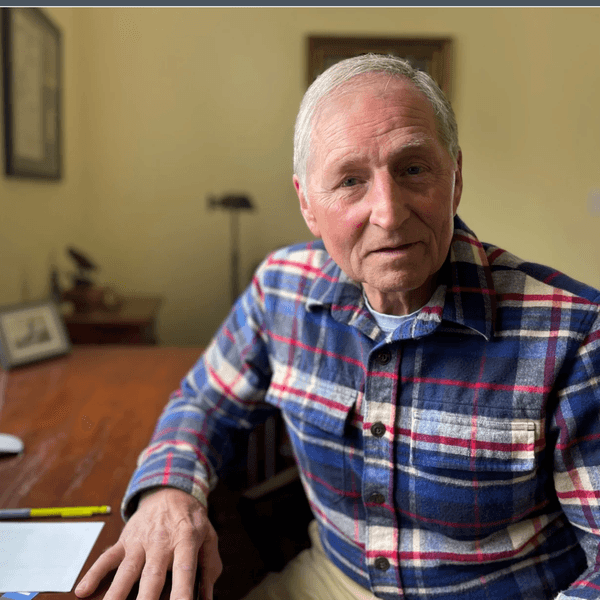
After 20 years of specializing in treating deadly skin cancers, the results published earlier this year were gratifying for Dr. Gerald Linette, a co-leader of the trial. But he urges patience to those looking for quick answers.
“(We) are still really the only lab that’s done this in people, and that’s three patients. I think that we have to be very cautious. Time will tell if this is going to work or not,” Linette said.
His partner in the trial, Beatriz Carreno, said genetic sequencing technology has sped the process of using mutations to encourage the immune system to fight cancer. They are now expanding the clinical trial to include more patients.
Brain cancer
Brain tumors are particularly challenging for immunotherapy targets because the molecules are more diverse compared to other cancers. And the immune system works differently in the brain than it does in the skin or other areas of the body. Messing with the immune system in the nervous system can lead to paralysis or brain damage.
Genetic sequencing creates a search party for “the Achilles heel in each patient’s tumor,” said Dr. Gavin Dunn, a neurosurgeon. A clinical trial is underway to test vaccines against the most deadly brain tumors, called glioblastomas. The first patient will get a personalized vaccine in the next few weeks.
Breast cancer
Dr. William Gillanders led a study in 2010 on a vaccine that used a target called mammaglobin-A, a protein that is expressed in most breast cancers. The vaccine proved to be safe in women who had late-stage breast cancer that had spread to other parts of the body. The women had previously received traditional surgery, chemotherapy and radiation treatments.
Close to half of the 14 patients who received the vaccine had no tumor growth after one year, compared to one-fifth of the 12 patients who did not receive the vaccine.
Michelle Ashby of O’Fallon, Ill., was one of the patients who received the vaccine after she was diagnosed with stage four breast cancer at age 40.
“I knew there needed to be more research on breast cancer and if the study didn’t directly give me benefit, I felt confident it would give benefit to my daughter and other people who are struggling with breast cancer,” Ashby said.
For the next 5 years, Ashby had no cancer recurrence. In August, doctors found some cancerous growth in her breast tissue and it was removed surgically.
“I have statistically beaten the odds of what was expected of my survival,” said Ashby, now 46.
That initial research on the mammaglobin-A vaccine will be expanded with more patients, and new clinical trials are open to test personalized vaccines for breast cancer.
“Now that we understand that there is this very dynamic interaction between the immune system and cancers,” Gillanders said, “a lot of people think that immune responses will be more effective” with personalized vaccines.
Drug companies are not enthusiastic about the idea of personalized medical care that would require a different vaccine for each cancer patient. But new biotech companies are forming to take this approach. Schreiber of Washington University is a co-founder of one of these companies, Boston-based Neon.
Schreiber said that in five years, scientists should have a good idea if cancer vaccine treatments will be ready for general use. A lot of evidence will be required to prove that the immune system can effectively kill off cancer.
Personalized vaccines can’t be mass manufactured for pharmacy shelves. But the process of making them can be streamlined, doctors say. The process that wasn’t even possible five years ago has now been expedited to a few months from genetic sequencing of a patient’s tumor to the injection of the vaccine. The work is a classic example of moving basic science out of the laboratory and into the doctor’s clinic.
The looming question is what happens next. Dunn, the neurosurgeon who specializes in the deadliest type of brain tumors, said he believes in the basic science behind cancer vaccines.
“I really want to be measured about the expectations because we just don’t know yet,” he said. “But I’m an optimist by nature, and I’m extremely hopeful that what we’re learning in cancer immunotherapy will really bring us to a place where we can help patients.”
(c)2015 St. Louis Post-Dispatch. Distributed by Tribune Content Agency, LLC.
Photo: National Cancer Institute via Wikimedia Commons