Researchers Reduce Inflammation In Human Cells, A Major Cause Of Frailty
From Mayo Clinic News Network, Mayo Clinic News Network (TNS)
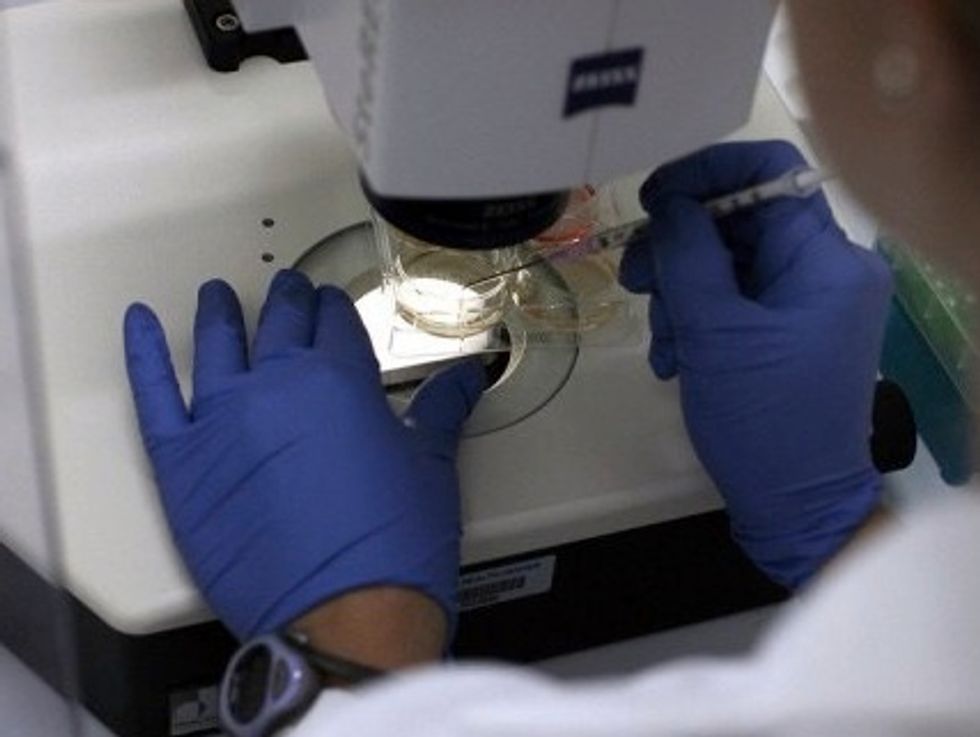
ROCHESTER, Minn. — Chronic inflammation, closely associated with frailty and age-related diseases, is a hallmark of aging. Mayo Clinic researchers have discovered that inhibiting key enzyme pathways reduces inflammation in human cells in culture dishes and decreases inflammation and frailty in aged mice.
The results appear in Proceedings of the National Academy of Sciences of the United States of America. While further studies are needed, researchers are hopeful that these findings will be a step toward treatments for frailty and other age-related chronic conditions.
In the study, researchers found that Janus kinase (JAK) inhibitors, drugs that work to block activity of JAK enzymes, decreased the factors released by human senescent cells in culture dishes. Senescent cells are cells that contribute to frailty and diseases associated with aging. Also, these same JAK inhibitors reduced inflammatory mediators in mice. Researchers examined aged mice, equivalent to 90-year-old people, before and after JAK inhibitors. Over the course of two months, the researchers found substantial improvement in the physical function of the aged mice, including grip strength, endurance and physical activity.
“One of the things we want to do is find some kind of treatment for this other than prescribing better wheelchairs or walkers, or other kinds of things that we are stuck with now that are Band-Aid solutions,” says Dr. James Kirkland, director of the Mayo Clinic Robert and Arlene Kogod Center on Aging and senior author of the study. A clinical geriatrician, Dr. Kirkland says he sees frailty in many of his elderly patients and that it’s often associated with poor outcomes and functional disability.
“Our goal is not necessarily to increase life span, and certainly not life span at all costs. Our goal is to enhance health span — the period during life when people are independent,” explains Dr. Kirkland. “This drug approach and others we are developing look like they might hold some promise in reaching that goal.”
©2015 Mayo Foundation for Medical Education and Research. Distributed by Tribune Content Agency, LLC
Photo: Mayo Clinic researchers have discovered that inhibiting key enzyme pathways reduces inflammation in human cells in culture dishes and decreases inflammation and frailty in aged mice. Researchers are hopeful that these findings will be a step toward treatments for frailty and other age-related chronic conditions. (Georg Drexel/Peter Atkins/Fotolia/TNS)