Uproar Over Fetal Tissue Affects ‘Under-The-Radar’ Lab
By JoNel Aleccia, The Seattle Times (TNS)
SEATTLE — As undercover videos released by anti-abortion activists roiled the nation this summer, sparking outrage directed at Planned Parenthood and re-igniting questions about the use of tissue from aborted fetuses, the Birth Defects Research Laboratory at the University of Washington quietly continued the work it has done for more than 50 years.
Since 1964, the Seattle lab has been a federally funded hub for the collection and distribution of tissues for research, obtained from miscarriages, stillbirths and abortions — including, recently, donations from a Planned Parenthood clinic in Washington state.
Few people outside of the scientific community realize that the lab exists, said Theresa Naluai-Cecchini, a research scientist at the site since 2011.
“We sort of fly under the radar,” she said.
But the tissues — fetal brain, liver, heart, kidney and other cells — long have been used at Seattle’s top science centers, as well as sites nationwide. Researchers at Fred Hutchinson Cancer Research Center, Seattle Children’s and the Allen Institute for Brain Science, among others, say the tissue has been crucial for local study of diseases and disorders as diverse as genetic heart defects, kidney malformations and macular degeneration.
In past decades, fetal cells were used to develop vaccines for diseases including polio, rubella and chickenpox, and they’re now being used in research of HIV, Alzheimer’s disease, autism, spinal cord injuries and other conditions.
“Our scientists learn so much from these fetuses,” said Stacey DiNuzzo, a spokeswoman for Seattle Children’s.
Local abortion foes say they’ve known for years about the UW lab and consistently have questioned the need to obtain the tissue.
“Obviously, we don’t object to research, but we do object to research from sources that we see as unethical,” said Dan Kennedy, chief executive at Human Life of Washington, the state affiliate of the group National Right to Life. “It is a gruesome, gruesome practice and we would urge all of those involved in it to get out of it.”
Fetal cells are prized for some research because they replicate rapidly and can adapt quickly to new uses. Federal law prohibits exchanging the tissues for profit, allowing fees to be charged only for costs such as transportation, processing and storage.
The UW lab, founded by Dr. Thomas Shepard, a pediatrician commonly regarded as the “grandfather of teratology,” or the study of birth defects, typically aims for a low profile. But controversy over covert videos released by the anti-abortion group the Center for Medical Progress, which prompted a congressional hearing last week, is having a chilling effect on the lab’s work, said Naluai-Cecchini.
In 2014, the lab collected 596 fetal samples from consenting women at two area hospitals and seven stand-alone clinics, and distributed 1,109 separate tissues to more than 60 researchers, Naluai-Cecchini said. The UW receives nearly $700,000 a year, including overhead costs, from the National Institutes of Health (NIH) to fund the lab, which has a repository of nearly 2,000 fetal samples from 370 individual donors.
Since July, when the videos surfaced purporting to show Planned Parenthood executives callously negotiating the sale of fetal parts, tissue donations have dropped dramatically, Naluai-Cecchini said.
“Most days, we have at least a single case to process,” she said. “Recently, we’ve had weeks where we’ve no tissue samples at all.”
The reason?
“I think that the women may hear that the clinics are profiting from the tissue,” she said.
The allegation had traction. Republican political leaders in several states called for investigations of Planned Parenthood’s practices. Cecile Richards, the organization’s national president, was summoned to testify before a congressional committee, where critics such as Rep. Jim Jordan, R-Ohio, called the videos “barbaric and repulsive” and accused the organization of seeking to make money from aborted babies.
Richards, however, said the videos were heavily edited to mischaracterize the organization and that Planned Parenthood facilities donate a small amount of fetal tissue nationwide and recover only processing expenses, as allowed by law.
That defense is echoed by Naluai-Cecchini, who said the UW lab charges researchers a flat fee of $200 a day to process and ship tissue. Last year the lab received a little less than $50,000 for those services.
“We don’t compensate the clinics for their tissue, and we don’t compensate the donors,” she said.
Fewer than 20 women agreed to donate tissue last year from among more than 3,000 who had abortions at centers run by Planned Parenthood of Greater Washington and Northern Idaho, according to spokeswoman Tanya Riordan. She declined to say which of the affiliate’s nine sites participated in tissue donation, out of fear that activists would attack the facilities, endangering patients and staff. The organization’s Pullman center was the target of arson last month.
Similarly, scientists at Seattle Children’s and Fred Hutch who use or have used fetal tissue in research declined to be identified individually, saying they fear they could be the subject of harassment — or worse.
But, through representatives, the scientists emphasized that the tissue is donated by consenting patients, including many who suffer miscarriages or who must end pregnancies because the fetuses have genetic defects or other problems.
Ed Lein, a researcher with the Allen Institute for Brain Science, said tissue from the UW lab was used in the reference atlas for BrainSpan, a unique resource that details the complete set of genes involved in brain development across the human life span.
“We recognize the extraordinary value of this precious resource,” he wrote in an email. “And our approach to creating high quality public data sets allows us to put important tools in the hand of thousands of researchers around the world.”
Naluai-Cecchini said she has personally worked with parents who find comfort in the idea of donating the tissue to help scientists find treatments or cures for the conditions that claimed their children.
“The couples desire something good to come out of their loss,” she said.
NIH expects to spend about $76 million on fetal tissue research this year, part of some $280 million allocated since 2011. But that’s a small fraction of the $581 million spent on human embryonic stem-cell research, and about $1.94 billion for adult stem-cell research in the same time period.
Some scientists say the need for fetal tissue research is waning, and that other techniques, such as using induced pluripotent stem cells or stem cells harvested from umbilical cords, offer more hope without the ethical problems of abortion.
Theresa Deisher, a Seattle molecular biologist who co-filed a 2010 lawsuit to shut down NIH support for embryonic stem-cell research, said the use of fetal tissue is “unnecessary — and it’s not useful.”
“Our research is dedicated to providing alternatives so that no one will feel compelled to work with that material,” said Deisher, president of Sound Choice Pharmaceutical Institute. She said she has worked with the Center for Medical Progress, the group responsible for the Planned Parenthood videos.
Researchers at Fred Hutch, however, said that in some cases — the environment of the fetal bone marrow, for instance — the cells can’t be replaced.
“In situations where other options are available, they are used, but fetal tissues have unique properties,” spokeswoman Rhonda Curry said in a statement on behalf of the scientists.
At the UW, Naluai-Cecchini said staffers hope the controversy wanes so that they can continue to concentrate on providing basic tools for research that may save lives.
“Every sample that comes through our doors is precious and valuable,” she said. “And they go to someone who wants to do something great.”
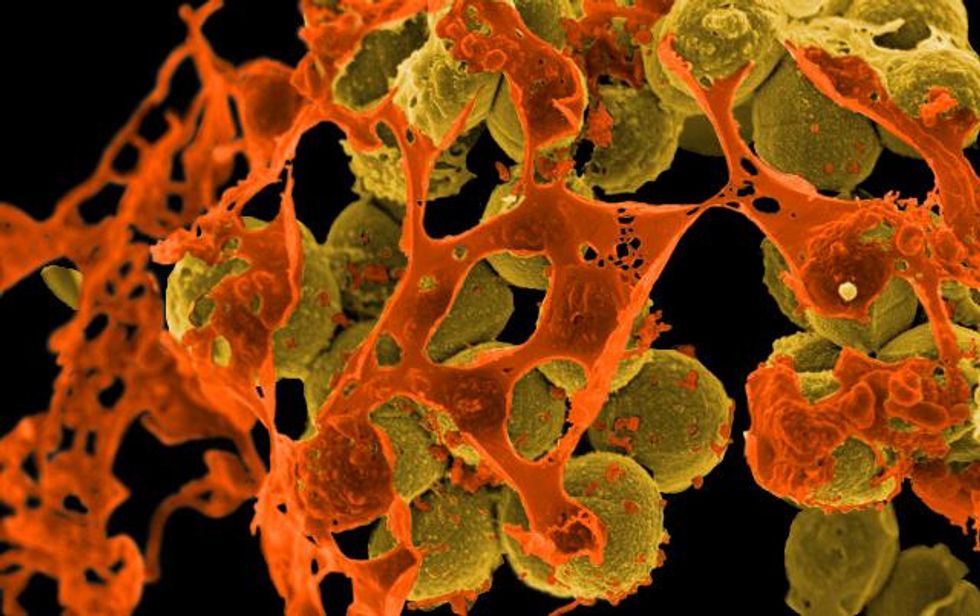
Photo: A Seattle research institution has been involved in fetal tissue research for decades. But due to videos attacking fetal tissue donation linked to Planned Parenthood, scientists at the organization are fearful that they will be targeted for harassment. Brendan Dolan-Gavitt/Flickr