Trump Van Winkle, Obamacare And The 'Money-Sucking' Health Insurance Industry
There is an old child’s tale about Rip Van Winkle. He fell asleep for 20 years and wakes up after the American Revolution and finds the world has changed in big ways. Donald Trump seems to be doing his own Rip Van Winkle routine. Yesterday, Trump suggested as an alternative to Obamacare, which he said feeds the “money sucking” insurance industry, that we just give money directly to people and let them buy their own healthcare.
This is a Rip Van Winkle story because Trump seems to think he has come up with a new idea. He apparently has missed the debate around healthcare reform that led up to Obamacare. He also apparently missed the debate on developing an alternative during his first term.While we don’t know exactly what Trump has in mind -- the plan will be ready in two weeks :), I hear -- there are fundamental problems with this sort of "just give people cash" idea. These problems push serious people, who have been awake, towards something like Obamacare or universal Medicare.
The basic problem of providing healthcare coverage is that some people have health conditions that are very expensive to treat, but most people are relatively healthy. If we just left things to the market, insurers will only cover healthy people. These people are very profitable for the industry, since they are basically just sending their insurer a check every month.
The problem is with the tens of millions of people who have health issues like diabetes, heart disease, cancer, or other conditions. These people are big money losers for the industry. They will avoid insuring them if they can or alternatively charge them tens of thousands a year for coverage. They may also contest making payments by claiming people had failed to disclose their health condition when they applied for insurance. I briefly went through the problems of the pre-ACA insurance market a few weeks back.
If Trump just gives people cash, it will do nothing to get around these problems. First, it is not clear which people he wants to give cash, and which cash. If he just means the enhanced subsides, he has around $35 billion a year to play with. Currently, around 22 million people get the enhanced subsidies, so that would imply checks of around $1.600 a year.
But there are another 28 million people currently without insurance, and another 2 million getting insurance in the exchanges without subsidies. Surely these people should be eligible for the Trump checks also. That would come to 52 million people sharing $35 billion, giving them each a check of less than $700.
Making the story even more complicated, people gain and lose coverage all the time, as they or a family member gets hired or leave a job with insurance. They may also gain or lose coverage for a government program like Medicaid. This means Trump has to figure out whether he will be sending out his checks once a year, giving many people a huge bonus and screwing those who lose their job after the cutoff date. Alternatively, this would have to be some sort of recurring payment, monthly or quarterly.
Perhaps Trump intends to take all the money going to Obamacare, not just the enhanced subsidies, which the Center on Policy Priorities puts at $125 billion, and roll it into his Trump checks. That would make them around $1,900 a year.
The next question is what Trump expects people to do with their money. A young healthy person may be able to cover their healthcare costs with $1,900 a year, but even these people would likely want insurance against the risk they may incur a serious illness or be in some sort of accident. Good luck finding insurance for $170 a month.
And the problem is far worse for older people and people with major health issues. In an unregulated insurance market, these people would be paying thousands of dollars a month for their insurance. Their Trump check will not go very far towards covering a premium of several thousand dollars a month.
Perhaps Trump plans to keep the Obamacare restrictions that require insurers to cover everyone, regardless of health condition, and prohibits discriminating based on health condition. That would limit the payments for people with health problems but still mean premiums that dwarf the size of the Trump checks, especially for those in the oldest pre-Medicare age bracket 55-64.
That would also put us basically where we are now except the checks would be smaller and untargeted, since all people without insurance, not just those enrolling in the exchanges, would be getting checks. Also, the current payments are adjusted by income. We don’t know whether Trump plans his checks to be income-based.
And in this story, the money would still be going to money sucking insurance companies, except presumably with less regulation so that the money sucking insurance companies could suck up more money. Under Obamacare, insurers have to pay out at least 80 percent of what they collect in premiums to providers, otherwise their customers get a rebate. Since Trump wants to get the government out of the picture, the insurers could presumably pocket even more money.
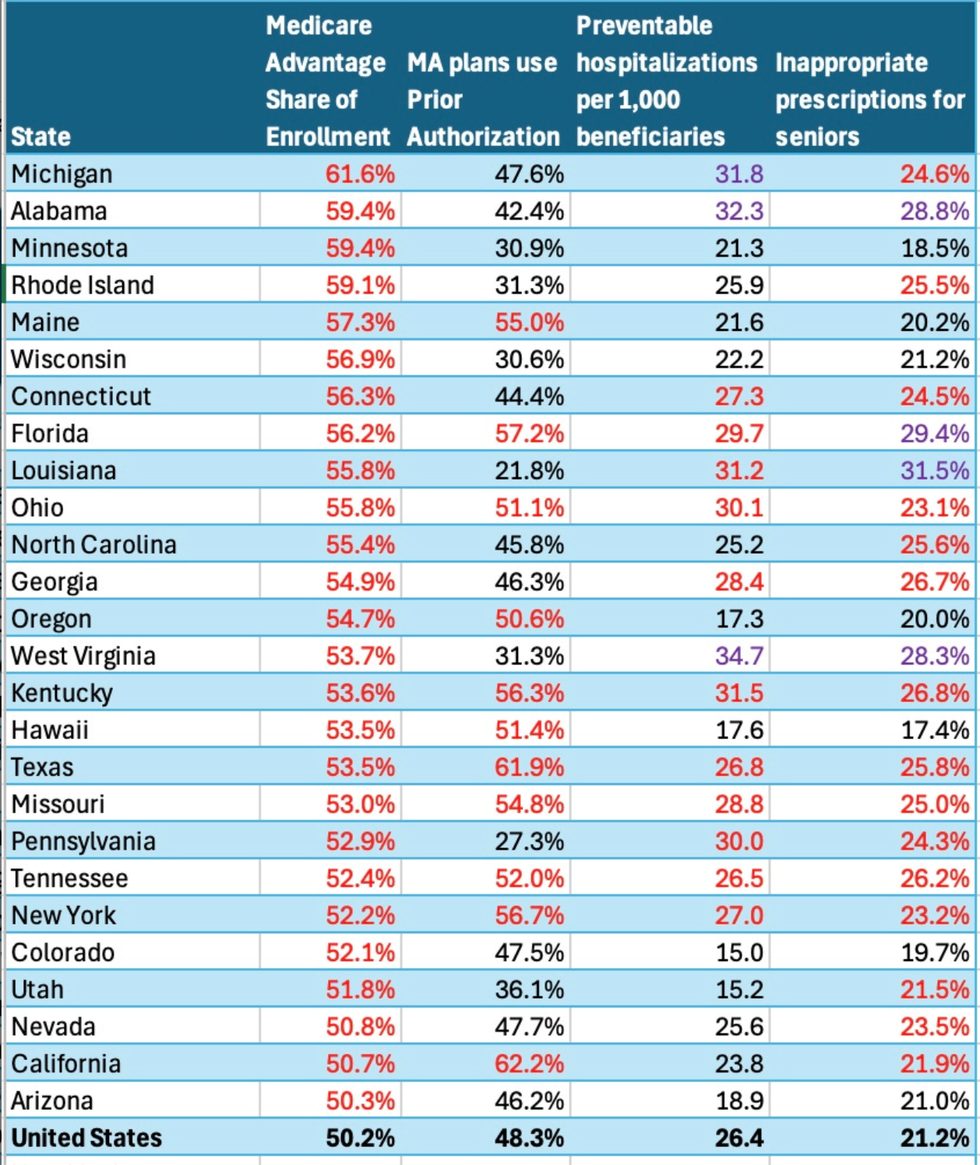
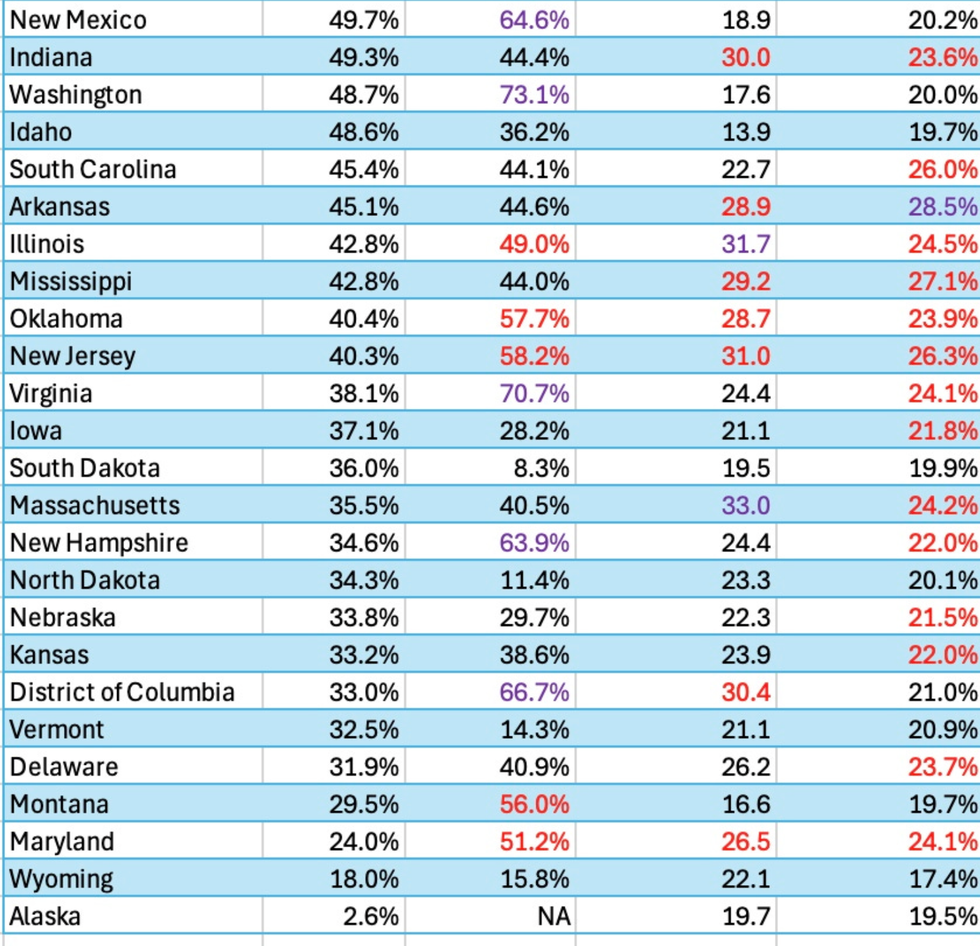
If Trump really wants to go after the money sucking insurance companies, getting them out of Medicare would be a great start. They mostly add cost to the program. He can improve the traditional program, adding dental, eyecare, and hearing coverage, and also imposing an out-of-pocket cap, and stop paying money sucking insurers in the Medicare Advantage program. Due to their higher administrative costs and profits, Medicare Advantage costs the government at least $100 billion a year compared to the traditional Medicare program.
If we’re really serious about cracking down on the money sucking insurance companies, why not go all the way and just provide universal Medicare. This would not only save the money directly paid to insurers, it would also eliminate much of the cost that hospitals, doctors’ offices and other providers have to incur dealing with complex forms from multiple insurers. This could save as much as $1 trillion a year ($8,000 per household) compared to what we pay now for administrative costs and insurance industry profits.
A universal Medicare system would also mean that everyone has access to healthcare regardless of where they work, what government program they qualify for, or if they remembered to pay their insurance premium last month. Not many would have expected Donald Trump to be the person to get us to Medicare for All, but if he really wants to crack down on money sucking insurance companies, that would be the way to go. Welcome aboard, comrade!