'Great Healthcare': White House Delivers Trump's Concept Of A Non-Plan
One year into his second term, President Donald Trump on Thursday called on Congress to pass a health care plan that would do next to nothing to lower employer-based insurance costs or reduce out-of-pocket expenses for individuals and families.
The 20-paragraph “fact sheet” on the administration’s plan contained few specifics; no new ideas; had only one estimate of projected savings or costs. Its insurance reforms included either provisions already on the books or previously rejected Republican proposals that would make things worse and force more people into the ranks of the uninsured.
The stock market took notice. Insurance stock prices (IHF) rose almost 2% on the news.
Its lead provision called on Congress to enact a law forcing drug companies to set prices at international levels. Given the pharmaceutical industry’s widespread support on Capitol Hill (most of the GOP and a hefty share of Democrats have routinely opposed so-called international reference pricing), passage of such a law is highly unlikely.
Moreover, the administration could do this on its own if it really wanted to. The first Trump administration in its waning days proposed a far-reaching rule for international reference pricing, which was rejected by the Biden administration in favor of pursuing price negotiations with manufacturers. Last month, it proposed two pilot projects that would apply international reference pricing to only 25% of Medicare patients, and then for only five years. The plan unveiled today made no mention of either effort.
Nor has the administration moved to expand rules over the drug prices it already has some say over — those for Medicare. The Medicare drug price negotiations law affected only a handful of high-priced drugs. The plan makes no mention of expanding that authority.
Financial markets took notice. Drug company prices (XPH) fell by less than 1% after the announcement.
The health care trade press was duly skeptical about the plan, calling it “a hodgepodge of health care policies that would create new price-control power over pharmaceutical companies, but that otherwise wouldn’t fundamentally overhaul America’s existing system,” as StatNews report opined.
Here’s what one investment advisory firm told its clients: “We view this new document as a largely political exercise. We think it is intended to demonstrate that the White House is doing ‘something’ about affordability and healthcare prices, but we believe the policies either stand little chance of being enacted by the current Congress or will have a minimal impact if enacted.”
The ‘details’
For drugs:
Beyond asking Congress to codify international reference pricing, the plan calls for making more drugs available as cheap over-the-counter medications. While this could limit sales of a few prescription anti-acids and pain relievers, for which there are already plenty of cheap over-the-counter alternatives, it would have no impact on the high prices of biotech specialty drugs, which are the major drivers of escalating pharmaceutical spending.
Nor would it affect the slow progress in bringing biosimilars to market, or their pricing. Most biotech drugs are either injected or infused in clinical settings, which makes them inappropriate for over-the-counter sales.
The plan also calls for Congress to end the kickbacks pharmacy benefit managers receive from large drug companies for including their products on preferred drug lists. The CBO estimated the GOP bill that passed the House in December with this reform would save drug insurance plans about $15 billion a year, a tiny fraction of the more than $300 billion that patients and their insurers spend at retail pharmacies each year.
For health insurance premiums:
The plan calls for scrapping the existing subsidy system for Obamacare plans and replacing it with a voucher that allows people “to buy the health insurance of their choice.” This refers to the GOP-backed Lower Health Care Premiums for All Americans Act (H.R. 6703), which would expand association plans that don’t meet basic Obamacare requirements like providing essential benefits or setting limits on out-of-pocket expenses.
The White House fact sheet touts the Congressional Budget Office estimating the association plan proposal would save $36 billion for the federal government. It didn’t mention the CBO’s conclusion it would cause 100,000 people to drop existing coverage each year over the next decade while adding just 700,000 newly insured through inferior association plans.
The White House plan also calls on insurance companies to publish the percentage of their revenues paid out in claims versus overhead and profit costs. The Affordable Care Act of 2010 already limits insurers, both on the exchanges and in the private market, to paying out at least 85% of the revenue in medical costs for large company plans and 80% for small businesses.
If there’s a problem, it’s in enforcement, not the standard. Indeed, I would like to see a 90% medical loss ratio as the best way to limit insurance industry marketing spending.
For providers:
The plan includes nothing about limiting hospital pricing; enforcing antitrust rules in every health care sector; or rectifying pay inequities between primary care physicians and specialists. Instead, its sole approach to addressing provider sector pricing is greater price transparency, which is already required by a rule adopted by the Centers for Medicare and Medicaid Services in 2019.
That has been a bust for two reasons. First, hospitals post those prices on websites or in places where consumers can’t find them or in such complicated tables that the average person has no idea what they mean.
But more importantly, even if prices were published in an easy-to-read format and posted on a wall, as the plan proposes, what would mean to most people? An analysis by the Health Care Cost Institute of the 70 most shoppable services (routine procedures like colonoscopies or cataract surgeries, for instance) accounted for just 12% of health care spending.
To sum up: When it comes to health care, affordability is most Americans’ number one concern. The plan the Trump administration announced Thursday does almost nothing to address that problem.
Merrill Goozner, the former editor of Modern Healthcare, writes about health care and politics at GoozNews.substack.com, where this column first appeared. Please consider subscribing to support his work.
Reprinted with permission from Gooz News


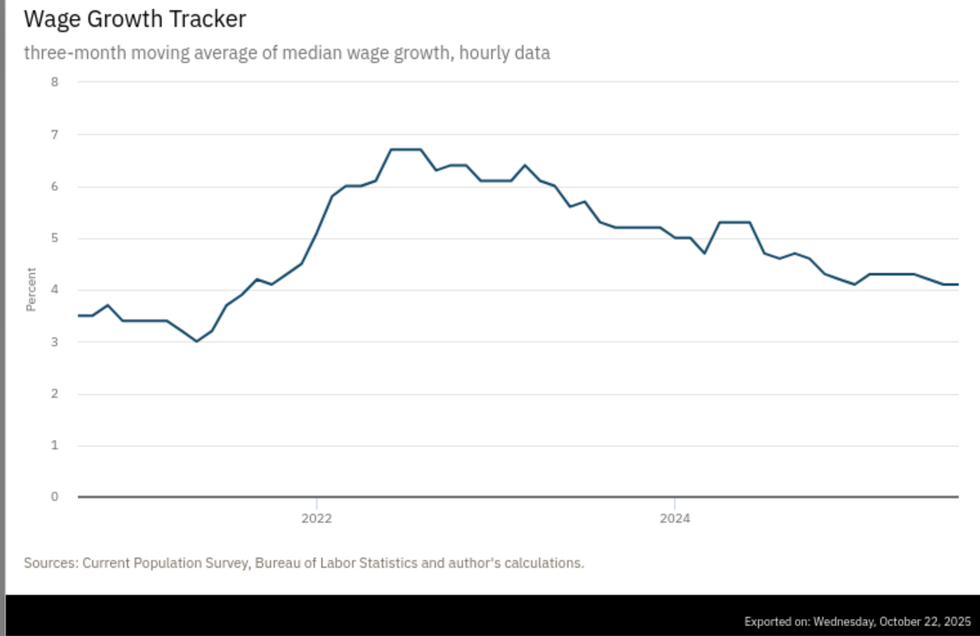 Source: Atlanta Federal Reserve
Source: Atlanta Federal Reserve